BY SAM SPOKONY | According to 2008 data published by the Centers for Disease Control and Prevention (CDC), there were approximately 56,300 new HIV infections in the United States in 2006. That number has remained relatively steady since the late ’90s, and has actually increased overall since the early ’90s, when new infections reached a low of around 50,000 per year.
“It’s such a striking statistic,” said Dr. Roy Gulick, (director of the Weill Cornell Medical College HIV Clinical Trials Unit). “To a lot of people, it means that HIV prevention efforts have not been working. In particular, the group we’ve seen a significant increase in recent years has been young gay men. So it’s become clear that we need new and specific strategies to help them prevent themselves from being infected.”
The promising future sought by so many medical professionals who are combating the AIDS epidemic may lie in the research and development of pre-exposure prophylaxis (PrEP). An outgrowth of post-exposure prophylaxis (or PEP, a short-term antiretroviral treatment that has been used since the early ’90s to decrease the likelihood of HIV infection after exposure to the virus, either occupationally or through sex), PrEP is a similar antiretroviral “drug cocktail” that could be taken (and in some cases, already is being taken) by HIV-negative men in order to help prevent them from becoming infected (seroconverting).
PrEP breaks ground in landmark efficacy study
A recent sense of optimism surrounding PrEP was a result of the Chemoprophylaxis for HIV Prevention in Men study (also known as iPrEx), a Phase III clinical study — sponsored by the National Institutes of Health (NIH) through a grant to the J. David Grant Institutes at the University of California at San Francisco — that began in July 2007 and was published in the New England Journal of Medicine of November 23, 2010. The iPrEx study focused on 2,499 sexually active men who have sex with men and transgendered women who have sex with men — all of whom were HIV-negative at the time of enrollment. The study’s experimental group received a PrEP treatment — a daily tablet that combined 200 milligrams of the drug emtricitabine, or FTC, and 300 milligrams of the drug tenofovir (a combination known by the brand name Truvada) — while the control group received a placebo.
In all, 100 cases of HIV infection occurred among participants in the iPrEx study. Thirty-six infections occurred among the 1,251 participants who were chosen to receive Truvada, while 64 occurred among the 1,248 participants who had received the placebo. Based on those numbers alone, PrEP was approximately 44 percent effective in preventing seroconversion.
While 44 percent efficacy might not be seen as wholly significant, what created perhaps a greater stir among researchers was analysis of the infected members of the experimental group. Blood tests revealed that, of the 36 men receiving PrEP who had seroconverted, 33 had no traces of the drug in their body prior to their positive HIV tests. This data presented a startling result: if the subjects who were supposed to have been taking Truvada daily — but were apparently not — were not counted, the efficacy of PrEP treatment rose from 44 percent to more than 90 percent.
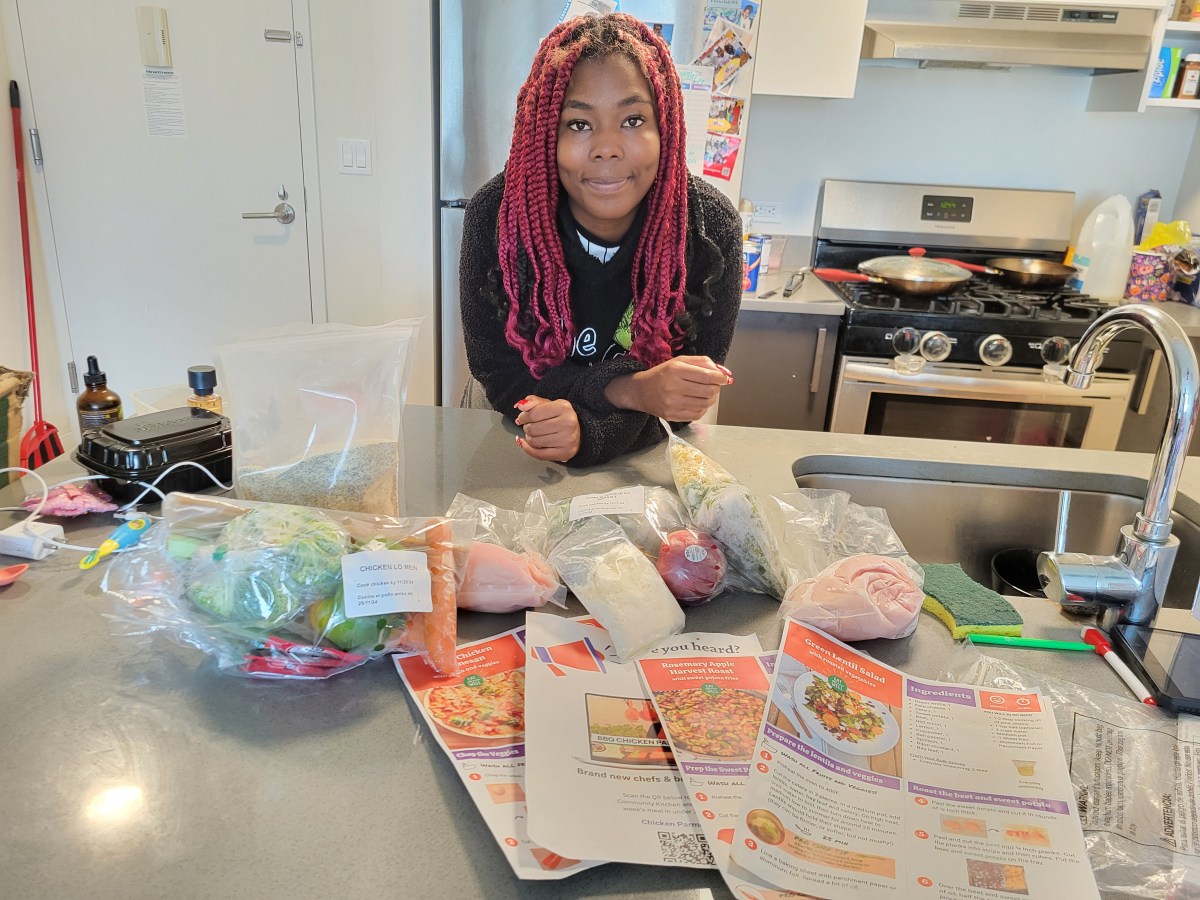
GMHC forum highlights adherence, access
Questions regarding the future of PrEP — as well as the issue of adherence to a daily treatment plan, which created such a wide variation in the overall iPrEx results — were the focus of a June 28 community forum at the Gay Men’s Health Crisis (GMHC) — (446 West 33rd Street). The forum, which was moderated by Dr. Sean Cahill (GMHC’s Director of Public Policy, Research and Community Health), featured four guest panelists: Kali Lindsey (Senior Director of Federal Policy for Harlem United), Dr. Kenneth Hugh Mayer (Medical Research Director for Fenway Health in Boston, Massachusetts), Ivan Monforte (Community Health Specialist for GMHC) and Mitchell Warren (Executive Director for the AIDS Vaccine Advocacy Coalition).
Mayer, who was a principal investigator in the iPrEx study, addressed the issue of adherence to a PrEP treatment plan early and often in his speech — especially as part of behavioral education that, within the gay community, has worked tirelessly to stress both safer sex practices (such as condom use) and rigid treatment regimens (like that of PEP).
“The way you try to think about ending any epidemic is by altering the source of the infection, altering host susceptibility and changing behavior,” he said. “But with HIV, I think that separating those into three different boxes is inappropriate, because behavior actually permeates everything. PEP isn’t going to work if you don’t take it.”
Mayer also touched on possible reasons for the trouble with daily adherence to Truvada in the iPrEx study. Side effects of tenofovir include kidney problems and changes in bone mineral density — but at levels that were not significant enough, in the study, to warrant any discontinuation of the drug. The most common and bothersome side effect, he noted, was nausea (which occured in about nine percent of the men in the experimental group).
“Recognizing that is really important,” Mayer stressed, “because if a person wants PrEP, they should be prepared for the fact that they might get queasy when they first start taking it. It’s not always without symptoms.” He concluded by stating that, because of new and ongoing studies, there would be enough data within the next year to hold a definitive study on the efficacy of a rectal gel that could potentially be used as a PrEP alternative.
Warren, in his time to talk, reminded the public that recent strides in PrEP development are not yet a cause for celebration, but for reflection on how medical experts should be translating research into results. He highlighted the fact that the last product for HIV prevention to be approved — or even reviewed — by the FDA was the female condom (in 1993). “We’ve done pretty badly,” Warren said, “not just in creating new options, but delivering the things that we’ve got.”
But he acknowledged that the recent cascade of PrEP results have entirely changed the landscape of medical knowledge, public safety and the possibility of ending the AIDS epidemic. What must come next, Warren declared, is finding the most direct and efficient ways to put those findings into practice.
“Who needs PrEP? Who wants PrEP? And who gets PrEP? The answers to those questions are often different, because the people who we may identify as the most need it, are not necessarily the ones who most want it — and those who most need it are often the ones who can’t get it.”
Insurance will play a role in drug distribution
With that in mind, Lindsay spoke very directly to the potential of receiving PrEP through health care providers — and the difficulty many high-risk gay men may have in receiving it as part of their health care coverage, if it becomes approved for HIV prevention by the FDA (which has not happened yet).
“1.1 million people in the U.S. are living with HIV, and about 18 percent of them are getting their health care through private insurance,” said Lindsay. “So the overwhelming majority of individuals who will want to access PrEP will be doing do through public health care programs. It looks like there may be some consideration from the Centers for Medicare and Medicaid Services in terms of paying for PrEP to get it to those at increased risk of infection, but we don’t have any of that in writing yet — and so nothing is currently insured.”
Before and after the panelists’ speeches, Chelsea Now spoke with a gay man, Len, who attended the forum and has been taking PrEP for over three months.
“So far, I’ve still been testing negative and there haven’t been any side effects,” he said. “My doctor even told me that there would be more side effects, but it’s been nothing. Zero.” Len did not give his last name because of that fact that his insurance provider is currently covering his PrEP plan. He did not want to be identified because, as previously stated, any HIV treatment drugs that might be used for PrEP have not been approved be the FDA for prevention, and thus will not be covered if an insurer knows that its client remains HIV-negative.
In the end, just another tool in the arsenal
In a July 6 phone interview, Dr. Perry Halkitis, Professor of Applied Psychology and Public Heath at New York University, told Chelsea Now that, although there is much to be excited about regarding PrEP research and development, it is much too early to declare the drugs capable of working solely on their own in an expanded, real world setting.
“I think that we’re still in an unclear place about where this going,” he said. “I know that the CDC is currently considering the findings from iPrEx — they want to determine how these findings will apply to real life. But that translation from experiment to real life is incredibly complicated, and we need to do implementation studies before we make any decisions.” Halkitis also made it very clear that, in his opinion, it would be a grave mistake, in the conversation surrounding PrEP, to forget the strides made in safer sex education and social interventions that have developed within the gay community over decades.
“There is this mood to replace behavioral with biomedical — and that’s the wrong answer. The PrEP findings are strong and favorable, but you can’t expect biomedical results to work on their own. I’d definitely consider the implementation of PrEP, but it has to be coupled with behavioral programming. That’s how it’ll yield better outcomes.
For more info on GMHC, visit gmhc.org or facebook.com/GMHC446. For detailed results of the iPrEx study, visit iprexnews.com/studyresults/english.html.