By Anindita Dasgupta
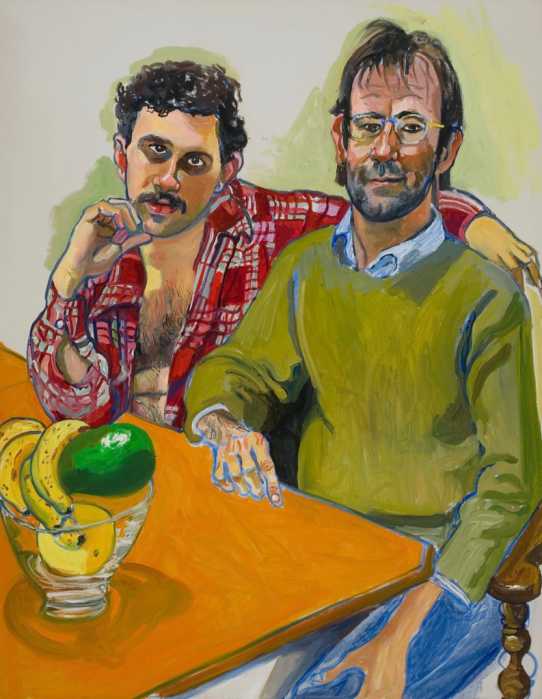
Twenty-five years since the onset of the AIDS pandemic, many gains have been made in combating the disease. Yet, the struggle is hardly over.
Since June 5, 1981, when the first cases of pneumocystis were reported in Los Angeles among gay men, the medical community has made vast advancements in treatment of the 1 million Americans estimated by the Centers for Disease Control to be living with H.I.V. While there is now federal funding for Americans to receive drug treatment, multipronged treatment approaches and rapid H.I.V. testing (test results available 30 minutes after testing), public health specialists maintain that finding a cure for AIDS is still a long ways off.
Dr. Marjorie Hill, executive director of Gay Men’s Health Crisis, said many factors have contributed to the ongoing AIDS crisis.
“Twenty-five years into the epidemic has taught us a painful lesson: H.I.V. is not just about H.I.V. and never has been,” she said. The majority of men diagnosed with AIDS are gay, at 67 percent, according to C.D.C. African-American males are also disproportionately represented.
Hill said the epidemic is fueled by racial injustice, homophobia and heterosexism. Until a cure is found, she said, one of the best cures is education and access to resources.
Dr. Jane Simoni, a professor at the University of Washington, has done research on victimization, substance use and H.I.V. risk behaviors among gay, bisexual and heterosexual populations in New York City. She credits gay men for their resilience in the face of adversity when the first cases were found.
“It could have been a time when they turned on each other or went back into the closet,” she said.
The adversity, Simoni was referring to, was the political climate in existence in the 1980s. The Reagan administration barely acknowledged that AIDS existed until a press conference four years into the epidemic, when Reagan finally used the term “AIDS.”
“Think back to 25 years ago,” Hill said. “Whether it was the federal government, state government or city government, to a large measure they were silent. Part of the reason for that silence was because it was a gay disease and government was silent regarding gay/lesbian issues.”
Today, government has not only acknowledged the problem, but funding has been put in place to aid those in need. Jeffrey Hammond, spokesperson for the New York State Department of Health, said the department has supported H.I.V./AIDS initiatives “at record funding levels currently totaling more than $2 billion in state and federal dollars annually; the largest funding commitment of any state in the nation.”
However, some activists feel that while state funding is more than what was available 25 years ago, a lot is left to be done to deal with social stigmas contributing to the disease.
Donald Grove, a data consultant with harm reduction programs who was involved with the 1997 National Syringe Exchange Survey, explained how some social stigmas and cries for identity among the gay community may have contributed to behavior leading to individuals becoming H.I.V. positive.
“We aren’t offered in our culture, any way to be gay,” he said. “I do whatever I need to do, to claim my gay identity.”
Grove cited the early 1980s and ’90s as a time when the general identity of being gay was partying and a promiscuous lifestyle, leaving young gay men wondering, “What’s wrong with me? I’m not promiscuous enough!”
Promiscuity, in part, led to the spread of diseases, among them H.I.V. Grove said there must be more discussion about identity, sex and sexuality, “so they can come up with their own concepts of who they are.”
Current research suggests that in addition to social pressures that may encourage promiscuity, drug use plays a role in the occurrences of H.I.V. and sexually transmitted diseases in gay men.
Dr. Alan Clear of the New York City Harm Reduction Coalition said, “It is well documented that gay men have high uses of drug and alcohol.”
Recently, public health officials have found high numbers of crystal meth users who are also H.I.V. positive.
Grove talked about his own experience with crystal meth: “It made me feel better about myself,” he said. “But I would feel so rotten after.”
In addition to the euphoria from crystal meth, users cite the drug’s powerful effect on the libido. Clear explained that the form of crystal meth popular among users today also contains a “Viagralike component” allowing men to sustain erections for prolonged lengths of time.
Dan Carlson, of the H.I.V. Forum, explained that as a result of these effects, among gay men, crystal meth is mostly used in the context of sexual behavior. The concern among public health officials is that crystal meth users may not only contract or transmit H.I.V. through unprotected sex after taking crystal meth, but also through used syringes. (Meth can be snorted, taken anally or injected, the latter known as “slamming.”) As a result, many activist groups in New York City support syringe exchange programs under which users are supplied with clean syringes.
Grove explained, “In syringe exchange, what we work on is addressing what people are doing and not what people ought to be doing.”
Hill reinforced Grove’s statement by saying, “Needle exchange makes logical sense…and has saved thousands of lives.”
“Let’s deal with what you’re asking for when you walk in the door,” Grove said of crystal meth users. “Their sexual behavior is not the only problem in front of them.”
Current regulations state that syringe exchange programs can be made available if a population in a community wants one to exist; the programs must first be approved by the local community board.
Hill described further concerns for gay men in terms of H.I.V. in the future. She worries that with the presence of more effective medicines for dealing with H.I.V., the younger generation of gay men will not have the constant physical reminder that older generations may have had.
“While H.I.V. is no longer a death sentence, as it was for many people 25 years ago, and that’s a wonderful thing, there are still people dying from AIDS,” she said. “There are still people who are becoming H.I.V. positive because they haven’t received the information and support to stay H.I.V. negative.”
Indeed, medications have advanced further than A.Z.T., and what is considered “monotherapy,” or the use of one drug to treat the virus. Today, Highly Active Antiretroviral Therapy (HAART) is used as what Simoni called a “multipronged” approach to attacking the virus and bolstering the immune system.
However, while the number of people dying from AIDS has decreased in the last 10 years, the infection is still quickly spreading. Simoni explained that even though H.I.V. drugs today make living more manageable than before, they are still not cures, as anyone forced to take the medications for the rest of their lives can readily attest.
“Talk to anyone of them,” she said. “They’ll tell you they are not easy to take.”