In the world of healthcare, billing and coding, including matching the right codes from around 72,000 to the right services, is crucial for providers to be paid. Historically, it involves tedious work, resulting in numerous initial denials that can delay or prevent payment.
While AI in healthcare is changing everything from detection to diagnosis, the AI revolution has reached healthcare billing and coding. Manhattan- and New Jersey-based Med Science Data, for instance, says it speeded up the process by months and significantly reduced, if it didn’t entirely eliminate, errors.
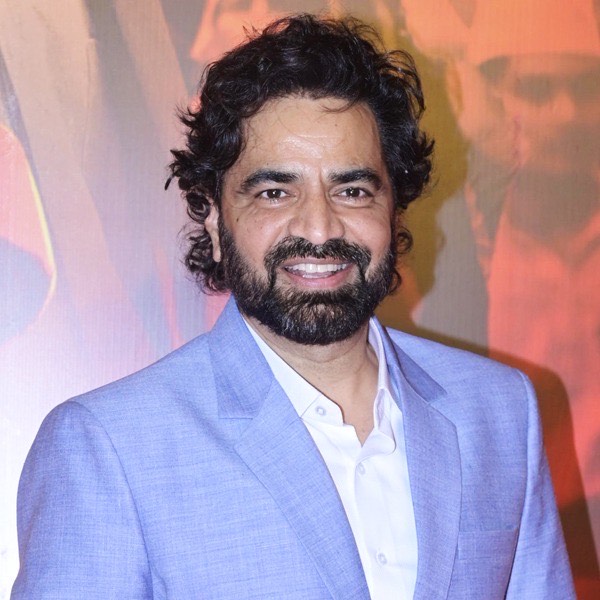
“Doctors, hospitals and clinics don’t have to suffer so much to get money from the insurance company,” said Med Science Data President Jay Patel. “Everything is so precise, accurate and crystal clear. It’s a good ecosystem for healthcare.”
As part of a behind-the-scenes AI revolution beyond detection and diagnosis, Med Science Data and other companies using AI to code and bill are increasing efficiency in the final piece of the puzzle.
Med Data Science handles billing and coding across a wide range medical specialties to improve revenue cycle management, reduce administrative burdens, and ensure maximum reimbursement for services.
By handling complex insurance claims, the idea is providers can focus on patient care, saving money and time.
“Everything’s turned around super fast. Our AI does every thing faster and sends it right away,” Patel, who was recently named one of the Long Island Press’ Healthcare heroes, said. “It’s a very speedy process.”
Physicians and other providers said that AI can make coding and billing more efficient, making their life easier and improving reimbursement.
“Routine tasks are handled seamlessly, claims are submitted with unmatched accuracy, and denials have dropped significantly,” said Dr. Susan Szapiel, a neurologist using Med Science.
Dr. Hardik Ramani, a physical therapist in New York, said Med Science Data’s use of AI increased efficiency and speed. “Authorizations are tracked more efficiently, coding errors are virtually eliminated, and reimbursements come in faster,” he said in a written statement.
Patel said 20% of claims typically result in denials with traditional procedures, although Med Science sheared that to 7%, using computers and a coder to double check.

“You need a human. You can’t do everything 100 percent by AI. The AI model is very well trained. The results are really good,” Patel said. “We have a second set of eyes.”
Med Science Data, Patel said, examined hundreds of denials to figure out why and prevent them. It doesn’t share data globally, as might be done by companies based abroad.
“We do not send our data base anywhere in the world. Turnaround time is quicker,” Patel said. “It’s a U.S.-based company.”
He added that patients benefit, because denials can lead to difficulties and prevent providers from offering service.
“The doctor won’t say we can’t take you because the insurance isn’t working,” Patel said. “It’s beneficial for everyone, patients, clinics, doctors and even the insurance company.”
Med Science Data submits claims electronically to speed up reimbursement, identifying discrepancies, such as underpayments, denials, or unpaid claims, to maximize revenue recovery.
Jay Aslam, who helped develop Massachusetts General Brigham’s original medical coding AI system, told Healthcare IT News AI-driven coding will likely continue to revolutionize healthcare.
“Our vision is to apply AI to increase efficiencies and reduce cost in the U.S. healthcare system, starting with autonomous medical coding,” he said of coding by computers.
A white paper titled “How AI is Revolutionizing Medical Billing and Coding,” from the University of Texas at El Paso, noted coders traditionally manually process “vast amounts of paperwork,” reviewed complex patient records, and assign codes for billing.
“This process, while essential, can be time-consuming and prone to human error,” according to the paper. “AI-driven solutions are now stepping in to streamline these tasks, reducing billing errors, speeding up claims processing, and improving revenue cycle management. “
Patel said a big gap between coders, often based abroad, and providers, creates room for error.
“The people writing billing and coding have no idea about the surgery. So often miscommunication happens,” Patel said. “That’s why the insurance company isn’t satisfied and you have a denial. I want to take care of the gap, so everybody’s on the same page.”
Patel said a certain amount of denials is, if not inevitable, likely, since insurers may seek to deny claims to reduce payouts. But he believes efficiency can continue to drive down denials.
“We are happy with our results. Our denials are 7%,” Patel said. “I want to do less than 1%.”