The first thing microbes like fungi and bacteria must battle in order to thrive is not the humans to which they can be so deadly, but each other.
And left to their own devices, these microbes tend toward balance.
However, when humans have identified microbes as dangerous — like the bacteria that cause pneumonia in people, anthrax in livestock or leaf blight in crops — we’ve used chemicals and medicines to stymie those microbes.
So we’ve worked wonders to reduce the cost and difficulty of crop and livestock production, and to improve the health and lifespan of humans. But by depressing the population of microbial organisms humans are fighting, we also have eliminated competition for other microbes that are now on the rise, and we have pushed organisms toward mutations that make them resistant to our medicines.
A deadly fungus centered in NYC
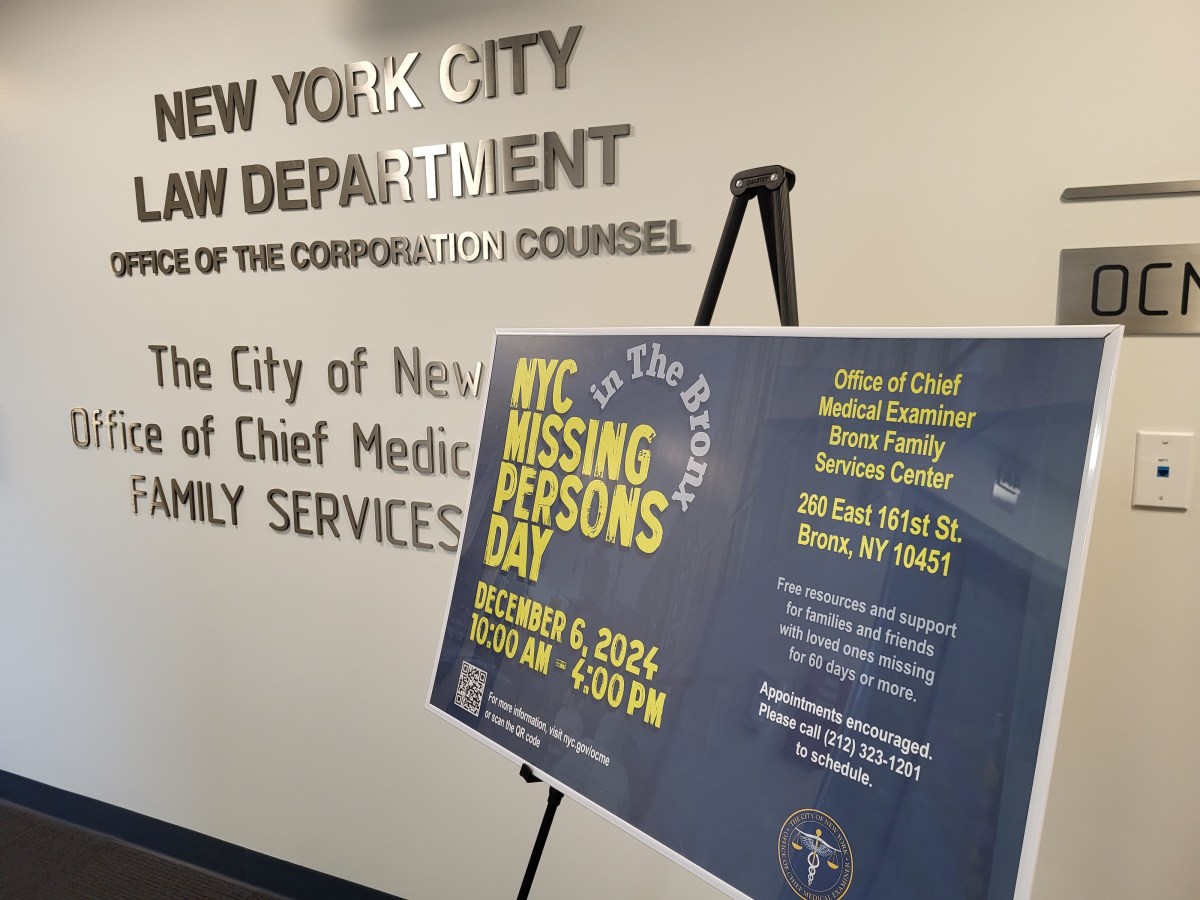
As a result, the nation faces new outbreaks. The deadly, drug-resistant fungus Candida auris, or C. auris, is centered in New York, difficult to eradicate and deadly. Practically nothing is being done to combat it, and hospitals and health departments won’t reveal where it’s been found.
Drug-resistant infections claim 700,000 lives a year worldwide. The most famous is known as methicillin-resistant Staphylococcus aureus, or MRSA, which infects about 90,000 Americans each year and kills about 20,000. It is highly resistant to a wide variety of antibiotic treatments.
Because of the prevalence of MRSA — and the spread of other antibiotic-resistant bacteria that can cause pneumonia, tetanus, typhoid fever, diphtheria, syphilis and leprosy — industrialized societies like the United States and Western Europe are realizing that pumping crop fields, livestock and humans full of antibiotics can lead to devastating results. Doctors are refusing to prescribe unneeded antibiotics. Patients are learning not to ask. And farmers in the United States have slashed the use of antibiotics in meat and milk by a third since the use of antibiotics to make animals grow more quickly was banned in 2017.
But the shift away from overuse of antibiotics is coming too slowly.
Doctors and government officials have worked for years to grapple with highly infectious bacteria that resist antibiotics and are tenaciously difficult to eradicate.
Their new worry, the drug-resistant C. auris, was first reported in the United States in 2017. About 600 instances of the infection have been diagnosed nationwide. More than 300 confirmed cases were in New York. The state Department of Health won’t say in which hospitals the fungal infection has been identified.
A devastating threat
The fungus first appeared in Japan in 2009. It carries a mortality rate of about 35 percent, is highly resistant to antifungal agents and nearly impossible to eradicate from a room once it arrives.
The New York Times reported that after a man died at a Brooklyn hospital in 2018, his hospital room had to be stripped down to the studs to eradicate the auris germ after everything in the room tested positive.
Drug-resistant infections are becoming one of world’s most devastating dangers. The response — in how we treat crops, livestock and human illness — must change. New treatments must be invented, and policies must be created to stop the excessive use of such products, and to inform people when and where outbreaks occur.
And so far, hardly anything is being done at all.