By Michael J. Dowling
Clearing the record on Center for Comprehensive Care
Since North Shore-Long Island Jewish Health System unveiled its plans to return healthcare to Greenwich Village with our Comprehensive Care Center, some have made wild claims about what this center will or won’t be in order to further their own causes or personal agendas. Below is our effort to set the record straight and explain in our own words why we feel this facility will provide exactly what the community needs.
Myth: It could take hours for a proper diagnosis at the North Shore-L.I.J. emergency department.
Fact: That’s entirely untrue. The emergency department will be staffed 24/7 by board-certified emergency physicians, as well as 30 specially trained nurses and other staff experienced in treating a wide range of symptoms and conditions. The E.D. will provide community residents with unlimited access to specialists, leveraging North Shore-L.I.J.’s vast network of physicians, who will be able to provide additional clinical resources to determine the best course of treatment. To ensure that patients’ conditions are properly evaluated and that safe, informed judgments are made before they are treated and discharged, the facility will feature around-the-clock observation through a clinical decision unit that provides clinicians the ability to follow patients for an extended period of time.
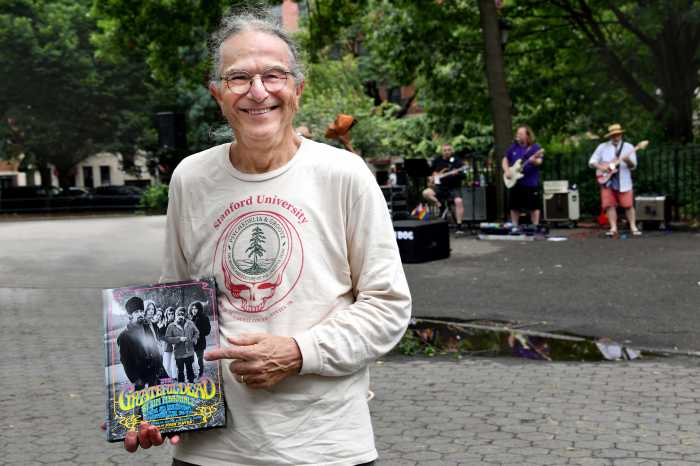
An exterior rendering of North Shore-Long Island Jewish Health System’s planned free-standing emergency department and comprehensive care center. North Shore-L.I.J. would gut-rehab and adaptively reuse the existing, six-story, landmarked St. Vincent’s O’Toole Building at 12th St. and Seventh Ave.
Myth: Free-standing emergency departments can actually drive up medical costs.
Fact: Actually, the opposite is true. North Shore-L.I.J. is proposing a freestanding E.D. to offer residents of the St. Vincent’s catchment area high-quality healthcare while reducing operating costs. Consistent with the recommendations of the New York State Commission on Health Care Facilities in the 21st Century (the Berger Commission), the state is looking for a new hybrid model of care that would meet community needs in the wake of a hospital closure. Furthermore, New York State regulations only allow the establishment of free-standing emergency centers when communities have been impacted by hospital closures.
Myth: Ambulances won’t take patients to the emergency department.
Fact: That’s an absurd scare tactic that is patently false. New York City’s 911 system will absolutely send ambulances to the Comprehensive Care Center and New York Fire Department leaders have indicated the value of having another E.D. to which they can direct ambulances and reduce wait times. North Shore-L.I.J. is working with the New York State Department of Health and the F.D.N.Y. E.M.S. to develop medical protocols based on the capabilities of the E.D. that we are planning at Seventh Ave. and W. 12th St.
While E.M.S. protocols dictate that patients experiencing a heart attack, stroke or a serious injury must be taken to a specialty-appropriate emergency department or trauma center, North Shore-L.I.J.’s proposed E.D. would have the ability to care for patients who are brought to the facility by a family member or friend trying to find help. Under those circumstances, the patient would be evaluated, stabilized and then transported to the closest appropriate facility, utilizing a North Shore-L.I.J. ambulance stationed at the E.D.
Myth: Emergency medical technicians (E.M.T.’s) and paramedics will be forced to make decisions about what type of treatment patients need before they see a doctor.
Fact: The city has a sophisticated 911 system, with F.D.N.Y. E.M.T.’s and paramedics who are among the best-trained emergency professionals in the world. In addition to their training, most have many years of experience making rapid, life-and-death decisions regarding patients in need of emergency care. It’s a disservice to these professionals to suggest that they won’t know when their patients require the services of a Level 1 trauma center. What’s more, the emergency department proposed by North Shore-L.I.J. would be able to treat more than 90 percent of the conditions seen at the former St. Vincent’s emergency room.
Myth: The emergency department is an unregulated facility where patients without coverage can be turned away.
Fact: False. The emergency department will be licensed as a hospital emergency department as a division of Lenox Hill Hospital, and will meet all the same regulatory standards as on-site hospital emergency departments. Our facility will accept all patients, regardless of ability to pay, and provide subsidized care for uninsured and underinsured patients.
Myth: Patients who require hospitalization will automatically be taken to Lenox Hill Hospital.
Fact: That’s simply not true. The emergency department will provide rapid transport to an appropriate facility or to one of the patient’s choosing. An ambulance will be stationed at the emergency department to provide rapid transport of patients to a higher level of care when required. In addition, North Shore-L.I.J. will develop transfer relationships with Bellevue for major trauma, New York Presbyterian and Staten Island University Hospital for burn patients, and Beth Israel Medical Center, New York Downtown Hospital and Roosevelt Hospital for other services.
Myth: The emergency care that North Shore-L.I.J. can’t provide is the care that matters most.
Fact: Based on its experience running 14 other hospital-based emergency departments across the New York City metropolitan area, North Shore-L.I.J. expects that its proposed emergency department would be able to “treat and release” about 94 percent of patients. Again, while patients in the most dire situations must be taken to a trauma center or a specialty center, staff at the comprehensive care center would be able to evaluate, stabilize and then transport them to the closest Level 1 trauma facility or specialty center, utilizing a North Shore-L.I.J. ambulance stationed at the E.D. Having those critical resources available in a neighborhood facility will facilitate proper movement of patients along the continuum of care.
Myth: The emergency department will treat 40 percent fewer patients annually in a community that has doubled in size.
Fact: Actually, only about 23,200 residents living in the service area defined by the Community Health Assessment Steering Committee visited the St. Vincent’s emergency department in 2009. Of those, 19,410 (about 84 percent) were treated and released. The remaining 3,800 were admitted to the hospital for a variety of reasons. About half of those patients who were admitted came to the St. Vincent’s E.D. by ambulance, meaning F.D.N.Y. protocols would now result in them being brought to appropriate area hospitals, such as Beth Israel and/or Bellevue. North Shore-L.I.J. anticipates that its proposed E.D. would eventually receive about 30,000 visits annually, which would fill a major gap for local residents who now have to travel out of their neighborhoods to access emergency care and other critical healthcare services.
Myth: A new hospital can be built for a fraction of the cost.
Fact: No. Unfortunately, the economic realities of today’s shrinking healthcare landscape make it difficult, if not impossible, to open and operate a new full-service hospital anywhere in New York City. When St. John’s Hospital in Queens closed two years ago, North Shore-L.I.J. seriously explored the feasibility of building a new hospital nearby, but learned that it would need to invest about $2 million per bed to make the project a reality — the equivalent of $800 million for a 400-bed hospital.
Since St. Vincent’s announced plans in January 2010 to close, other hospitals and health systems have had plenty of time to formulate and present a plan to open an acute-care hospital serving that area. But North Shore-L.I.J. has been the only provider to step forward with a concrete plan to resurrect healthcare services to this community. The reasons are simple: the inability to secure financing and the absence of a need for more hospital beds in Lower Manhattan.
North Shore-L.I.J. has put forth an innovative solution that will address a critical aspect of the healthcare dilemma facing residents of Lower Manhattan.
In regard to the Coalition for a New Village Hospital’s claim that St. Vincent’s Coleman Building could serve as a suitable site for a full-service hospital, the coalition conveniently ignores the 2009 finding of the New York City Landmarks Preservation Commission, which concluded that St. Vincent’s Coleman and other buildings were “outdated,” “physically inadequate” and “in need of replacement.”
Dowling is president and C.E.O., North Shore-Long Island Jewish Health System