By Lincoln Anderson
To help returning Iraq war veterans deal with post-traumatic stress disorder, the Veterans Affairs Hospital is using a new technology: a virtual-reality simulator.
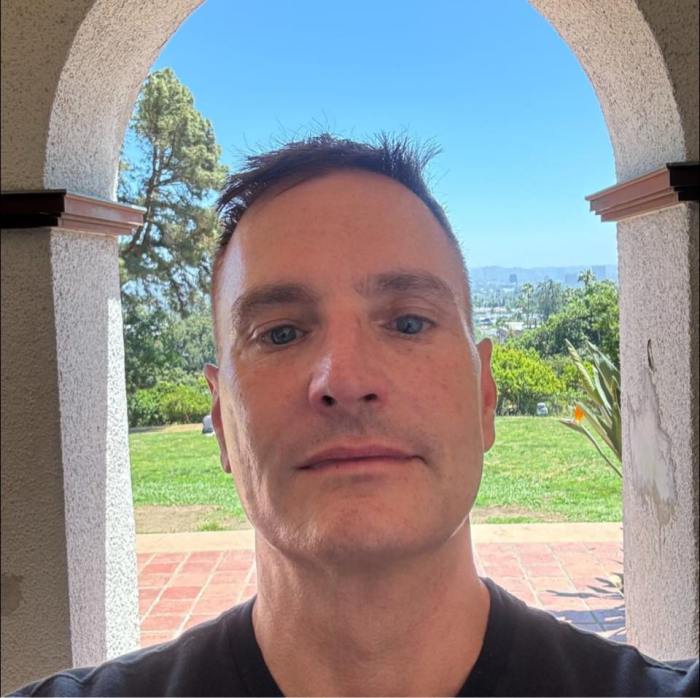
Michael Kramer, a clinical psychologist, is co-leader of the V.A.’s support group for returning Iraq and Afghanistan veterans. He’s experienced in virtual-reality P.T.S.D. therapy, having used it previously at Weill Cornell Medical College with 9/11 World Trade Center attack survivors. He was brought to the V.A. on E. 23rd St. to implement this new therapy for vets.
“We’re all struck, I think, in the clinic, at the level of traumatic exposure,” Kramer, 44, said of the patients he’s seeing. “People are spending a longer time on tour. There’s less time in between tours during which they can regroup.”
Also, similar to the Vietnam War, the nature of the conflict — no clear battle lines, fear that anyone could be an insurgent — creates a highly stressful situation.
“There’s no down time. There’s no safe space,” Kramer said. “You’re always on alert.”
The 17 clinical symptoms of P.T.S.D. include nightmares, insomnia, exaggerated startle responses, excessive irritability, detachment from others and flashbacks, among others. It’s common for it to break up marriages.
Specific to Iraq vets — who spent a lot of time in Humvees and vehicles on dangerous roads — are driving issues. According to Kramer, one of the more common themes among returning vets he’s seeing is that they want to drive in the middle of the road. In Iraq, improvised explosive devices, or I.E.D.’s, are often hidden on roadsides, where they can more easily be camouflaged.
“So now these guys are driving in the middle of the road,” Kramer said. “Intellectually, they know New York is not Iraq — that’s their human brain thinking. But by the time you think, ‘This is New York, not Iraq,’ there’s another part of your brain — the reptilian brain — that’s beaten you to the punch; it’s exceptionally fast.”
Luckily, the vets aren’t getting into accidents because they’re so hypervigilant. In some cases, they’re not driving — or are letting others drive, though that just adds to stress because one feels out of control of the situation.
Driving under bridges can cause panic, too, since in Iraq, insurgents sometimes hide underneath them, Kramer added.
Crowds can also provoke anxiety.
“Crowds are a dangerous place, in general,” he noted. “A lot of people who don’t go to war don’t like crowds. If you are hypervigilant, a crowd is not a place you want to be — because you can’t make everything safe.”
A normal person might take 30 seconds to recover from a stressful situation like a very loud truck backfire, after the brain processes that it’s not a dangerous situation. A veteran suffering from P.T.S.D., however, might take hours to recover.
Ultimately, while some people may be more susceptible to P.T.S.D., there’s one constant, according to Kramer: “The greater the traumatic exposure, the greater the likelihood that they will have P.T.S.D.”
The main P.T.S.D. treatment is exposure therapy — specifically, prolonged imaginal exposure, or P.I.E., in which the vet tries to call up the painful memories in order to gain some measure of control over them. Delving into the traumatic memories at first can bring up even more intense pain — but while the pain may never disappear, the anxiety can be lessened.
“You need to not avoid it — because by avoiding it, you keep it alive,” Kramer explained.
Some people aren’t that good at or comfortable with imagining, though, which is where the computer program, “Virtual Iraq,” comes into play.
The Manhattan V.A. is one of seven V.A. hospitals nationwide to have the new program, which costs $70,000. The program offers two scenarios: riding in a Humvee or walking around a typical Iraqi city.
The vet is seated, wearing a headset with virtual-reality goggles and can swivel his or her gaze 360 degrees and up and down to look around the computer-generated environment. He or she also wears headphones through which sounds, from the mundane, like a dog barking, to full-scale explosions, are heard. The platform on which the chair rests also can vibrate to simulate bomb blasts. The psychologist monitors all the action via computer screens.
The idea of the simulation isn’t to recreate exactly what happened to the vet, Kramer said. But the scenes are intended to be similar enough to get him or her to start talking about the traumatic experience. If it was a clear day when the incident happened, Kramer can make the scene clear. If it was night, he can make it dark. If there was a sandstorm, he can add a little sand — all through the use of the computer controls.
He can let the vet drive the Humvee, make him or her a passenger or add in a mounted machine gun, depending on what the vet was doing at the time of the incident.
Kramer can even introduce smells, through the use of eight small jars of oils with a variety of scents, which are blown toward the vet by a fan apparatus connected to the computer. Often the vets remember a certain smell right before a traumatic event occurred. The eight scents range from “Middle Eastern Spice Market,” to “Weapon Fire,” to “Body Odor.”
“It’s really vile,” Kramer said, offering a whiff of the “Body Odor” jar, “because there are people who spend 36 hours in a tank with other guys.”
As the vet walks or drives around the simulated environment, Kramer talks to him or her through the headphones, asking where the anxiety level is on a scale from one to 10. Gauging the patient’s state, he’ll use the controls to add, say, a Blackhawk helicopter flying overhead, a machine gun ambush or a random man yelling, “Go home, cowboy!”
But the psychologist has to be careful not to overdo it or produce the wrong effect at the wrong moment.
“You have to be in complete control of the environment,” he said. “If you hit the wrong key….”
Some veterans are too scared to try the computer program, fearful of its rekindling uncomfortable memories.
“A couple of them have looked at it and said, ‘No freakin’ way,’” Kramer said. “Their symptoms are severe and they don’t want any extra anxiety.”
Not surprisingly, though, the V.R. therapy is popular with young veterans, who have grown up playing high-tech home video games.
“There’s a certain coolness to this,” Kramer said, holding the purple control in his hand. “Young vets love this. Some of them might not come in if not for this.”
The V.A. has paid for three years worth of upgrades for the program. The next available option, for example, will include riding in a Humvee and having someone get killed in the neighboring seat.
Asked for his opinion on the war, Kramer said he does have one. But, as two V.A. public relations officials sat watchfully nearby, he said he couldn’t express it.